Regain control. Enjoy life again.
Deep Brain Stimulation
Dignity Health St. John’s Regional Medical Center is the only hospital in Ventura County to offer deep brain stimulation (DBS). DBS is a neurosurgical treatment option for patients with Parkinson's disease, essential tremor, dystonia, or other movement disorders who are not responding to standard medication treatments or are experiencing unwanted side effects of those treatments. During DBS surgery, electrodes are implanted within the brain to deliver electrical impulses. The stimulation offers patients relief from the tremors, rigidity, slowness of movement, and abnormal postures commonly seen in those conditions. The stimulation can be adjusted as a patient's condition changes over time.
Why Deep Brain Stimulation is Performed?
Neurologists may recommend DBS when a patient is not responding to standard treatments or is experiencing intolerable symptoms from those treatments.
Who can be evaluated for DBS surgery?
Patients who have the following conditions may be evaluated as possible candidates for DBS.
- Parkinson’s disease tremor
- Essential tremor (not due to Parkinson’s)
- Dystonia
Who is a Candidate for Deep Brain Stimulation?
Any patient with increasing loss of control of movement may be a candidate. The neurology assesses each case to determine candidacy.
What Happens During Deep Brain Stimulation?
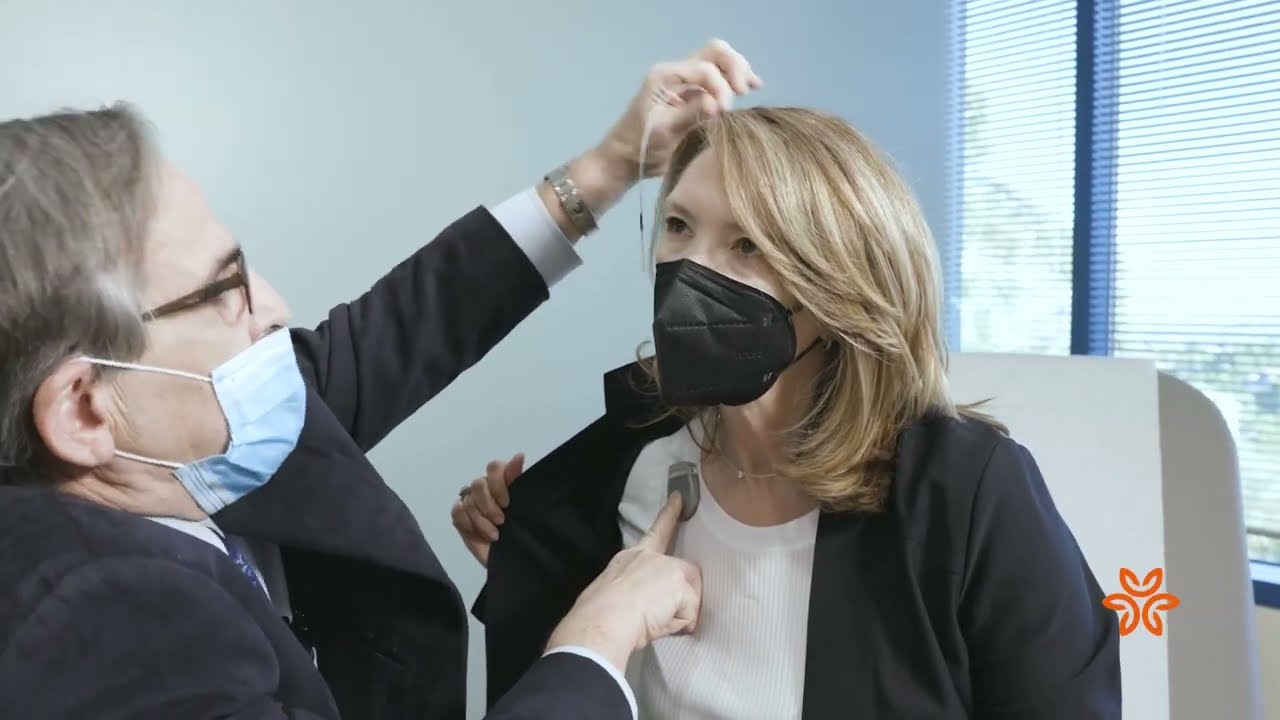
DBS is a two-step procedure. During the first procedure, a very thin lead (about the thickness of a strand of spaghetti) containing four electrode contacts is implanted into a specific target area in the brain. The lead extends through a small opening in the skull and is connected to an extension wire, which is connected to an impulse generator (battery or "pacemaker") that is implanted under the skin over the chest. Programming of the stimulation is easy and painless.
The surgeon is aided by computerized brain-mapping technology to find the precise location in the brain where nerve signals generate the tremors and other symptoms.
After 3-4 weeks post implantation, the battery is inserted and placed below the collarbone, similar to a heart pacemaker. The stimulators are turned on for the first time within a few weeks after battery implantation.
Deep Brain Stimulation Recovery
The average hospital stay following implantation of the DBS leads is 1 to 2 days. As for the second procedure, which involves placing the battery, most patients are able to return home on the same day.
Following both procedures, our surgeon will discuss what activities the patient should avoid during the recovery process. The patient will also be taught how to set the stimulator to control the pulse generator.
Multidisciplinary Team
Patients receive a comprehensive work up by a multidisciplinary team and the benefit of full modality therapy options, including acute rehabilitation for post-procedure fine motor programming. Our team includes:
- Movement disorders and other specialized neurologists who oversee the patient’s care
- Neurosurgeons who implant DBS hardware
- Physical medicine and rehabilitation specialists who support patients following DBS surgery
Meet Our Team
- Bradley Hiner, MD, Neurologist
- Akinwunmi Oni-Orisan, MD, Director of the Neurointerventional Program
Learn more about St. John's Deep Brain Stimulation Program
For more information about this groundbreaking procedure, please call (805) 988-7144.